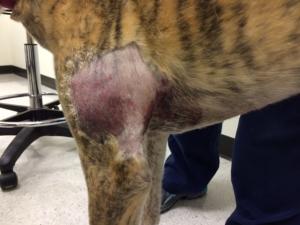
Orthopedic ultrasound? What a concept! Dr. Nele Ondreka DipECVDI, (http://www.sonopath.com/about/specialists/dr-nele-ondreka-dipecvdi), one of the world leading radiologists in orthopedic ultrasound, evaluated this case sent by Tomie Timon RDMS/RVT of Animal Sounds Mobile Imaging in Eugene, Oregon (http://sonopath.com/about/specialists/tomie-timon-rdms-rvt) through SonoPath Telemedicine. What’s going on with this bruised bicep/tricep region? Tumor? Bicep avulsion? Is it surgical? Is the joint involved? Is there bone lysis? All questions are answered when you team up a solid sonographer and solid interpreter half the world away. See the orthopedic ultrasound connection between Eugene, Oregon & Giessen, Germany that's all about a greyhound, a limp, a bruise, and a probe in this month’s orthopedic ultrasound June, 2015 case of the month.
Image Interpretation
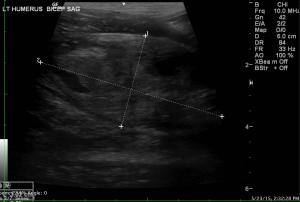
The muscle belly of the biceps was increased in thickness and appears shortened in length, but is contained within its fascial planes. The muscular tissue is hyperechoic in general. There is alteration of the fiber pattern and loss of the regular echotexture of the muscle. Color Doppler exam shows mild hyperaemia within muscular tissues of the biceps. The muscle belly measured 6.1 cm in length and 3.0 cm in thickness. There are two heterogenous lesions with a mass effect on the muscular tissue, but contained within the muscle belly. Within these lesions there is disruption of the regular fiber pattern and these lesions affect approximately 75% of the cross-sectional diameter of the muscle. The echogenicity of the lesions is predominantly hypoechoic, but there are anechoic cavernous areas contained within the lesions, which are color Doppler negative. There are also some hyperechoic foci with very mild acoustic shadowing present.
The proximal transition to the tendon of the biceps, the biceps tendon itself and its tendon sheath in the area of the intertubercular groove and the origin at the supraglenoid tubercle are not included in this study. The distal transition to the insertion on the radial head and medial coronoid process are not visualized either.There is a focal area of mild roughening of the bone surface in the cranial lateral aspect of the proximal humeral diaphysis. However, this is located in an area that bends away from the probes footprint. This area likely corresponds to the deltoid tuberosity, but a potential periosteal reaction cannot be entirely ruled out. The fatty tissue within the axillary area shows mildly increased echogenicity and some attenuation, but there is no separation of the fat lobule, which would indicate significant edema, but this is not present at that point. The axillary lymph node is prominent and measured 14 x 6 mm. The short to long axis ratio is preserved and still below 0.5. The corticomedullary definition and the fat in the lymph node hilus are preserved. There are no signs of vascular thrombosis within the imaged axillary vessels and the right auricular appendage does not show any abnormalities.
Sonographic Differential Diagnosis
The findings are compatible with a subacute partial rupture of the biceps affecting approximately 75% of the cross-section of the muscle belly with organizing intramuscular hematoma. There is a mild, generalized, subcutaneous and interfascial edema. Mild reactive hyperplasia of the axillary lymph node is likely associated with the resorption of the edema and hematoma. A spontaneous traumatic event is likely the underlying cause of the partial muscle rupture and hematoma formation. Neoplasia is a very low potential at this point, but there is a potential for further proximally or distally located lesions such as partial or complete ruptures of the biceps tendon. It is possible that these are within the proximal or distal tendinous parts or even avulsion fractures of the supraglenoid tubercle, radial head or medial coronoid process.
Outcome
A further work-up would include an ultrasonographic control examination within 7 days to monitor the progression of the organizing hematoma with the assessment of the proximal and distal insertion of the biceps tendon. FNA of the muscular lesion would only be indicated if the hematoma, limb swelling, or bruise does not show the expected rate of regression. The radiographs of the shoulder - and elbow joint if present - should be checked for further bony changes such as signs of traumatic bone injury i.e. avulsion fracture at the bicipital origin, osteolytic or osteoproliferative changes even if that is not very likely in this case. Shoulder joint stability should be clinically assessed. Rest, pain management and physical therapy for therapeutic management are recommended. Surgical options should only be considered in case of partial ruptures of the biceps tendon proximally, distally or in the presence of avulsion fragments.