Clinical Differential Diagnosis
(Lobetti):
Drug effects – iatrogenic Cushing’s disease, gastric ulceration, steroid hepatopathy, infectious disease from immune suppression, pancreatitis
Thrombo-embolic disease
Pre-existing causes for IMHA – neoplasia, bacterial/fungal infections, abscess, granuloma
Sonographic Differential Diagnosis
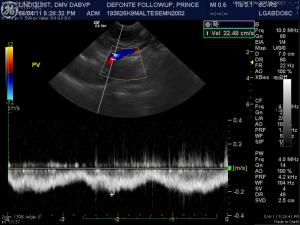
(Lindquist DMV, DABVP): Portal vein thrombus with secondary portal hypertension and ascites. Splenic thrombosis. Renal infarctions.
Outcome
The patient was treated with Plavix and a plasma transfusion after the first sonogram was performed. At a recheck examination several weeks later, the patient was found to be doing very well on current therapies. CBC and blood chemistry were both within normal limits. The patient was recommended to continue with the current protocol of Plavix, Prednisone, and Atopica







Comments