On Any Given Sunday: Meeting Sonographic Criteria For Intestinal Neoplasia But Neoplasia Doesn’t Win The Game. This is why we play the game…to ensure we don’t do “histopathological ultrasound” and not just call it neoplasia.
Patient imaged by Andi Parkinson RDMS and medical management by Dr. Pam Nesbitt, Surgery By Dr. Joe Zulty, Essex Middle River Veterinary Center, Baltimore, MD, USA.
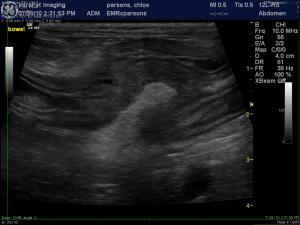
Sonogram: (G.I., 7/28/10): “Chloe”
History: (Kelly Vazquez,CVT): A 12-year-old FS Dachshund was presented at an emergency facility for intermittent vomiting and diarrhea lasting several weeks. The only obvious abnormality on physical examination was lethargy. She was treated Famotadine, Metronidazole, and discharged with a bland diet. At follow-up examination the following day at the RDVM, the owner reported that the patient had vomited twice and was having uncontrollable diarrhea. CBC and blood chemistry showed neutrophilia, lymphocytopenia, eosinopenia, elevated ALP activity, elevated CK, hyperamylasemia, and low TCO2. cPL was 173. Abdominal radiographs showed some loss of density in the cranial abdomen. The patient was treated with IV fluids, Metronidazole, Ampicillin, and Cerenia.




Comments
Special thanks to Dr. Zulty & Nesbitt for the virtual referral of this case by means of Andi Parkinson, RDMS of (Intrapet Imaging) and Chloe’s successful management.