Innocent murmur… I think not! Here is a case where acting on a heart murmur, no matter the age or grade, is a prudent choice in clinical practice. A young, rambunctious boxer was presented for an echocardiogram and ECG, for a low grade (1/6) heart murmur that had continued to be auscultated after several puppy visits to her veterinarian. No obvious clinical signs were present, other than panting, but not unusual for an exuberant puppy in a clinic setting! Many thanks to Dr. Shelly Knopsnyder of East Lane Veterinary Hospital and her awesome team in managing this case. SDEP-certified sonographer, Amanda Lacey of Animal Sounds NW provided the diagnostic images for this case study.
Sonographic Differential Diagnosis
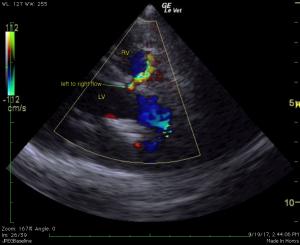
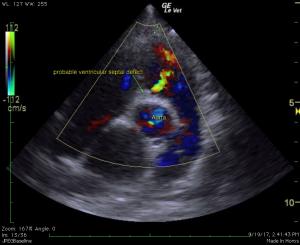
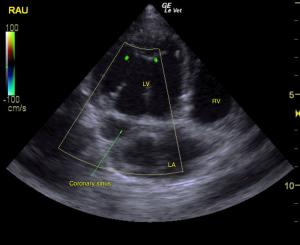
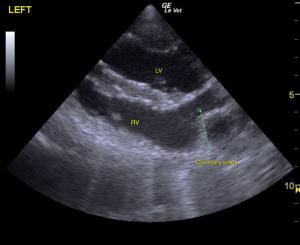
The murmur appears to be secondary to a small left to right shunting ventricular septal defect (~5mm), suspected restrictive physiology. Probable tricuspid valve dysplasia. Dilated coronary sinus (Ddx persistent left cranial vena cava vs. anomalous pulmonary venous return vs. other). Ventricular premature complexes. Possible high grade AV block during sedation (Ddx high vagal tone vs. myocarditis vs. idiopathic nodal fibrosis vs. other).
DX
Venticular septal defect.
Outcome
Placement of a 24-hour Holter monitor was advised to better assess the arrhythmia documented in the ECG, which is unlikely to be related to the VSD. If concurrent AV block and ventricular arrhythmias are diagnosed, a myocarditis may be present; in this case tick titers, protozoal titers, and potential for treatment with doxycycline would be indicated. The dilated coronary sinus may be related to a persistent left cranial vena cava or anomalous pulmonary venous drainage. A bubble study in the left cephalic vein would confirm the suspicion of a persistent left cranial vena cava. This is typically a benign congenital change. The lack of tricuspid regurgitation is a favorable finding. No cardiac medications appear indicated at this point, given the lack of clinical signs and lack of congestive heart failure on radiographs. With a small VSD the prognosis is typically good; recheck echocardiogram is 6-9 months was recommended. Due to the patient being clinically normal at home. as she was prior to the ultrasound, owners elected to not pursue further care except for recheck/echo/ECG that was recommended by the cardiologist.