Clinical Differential Diagnosis
Gallbladder - cholecystitis, mucocele, rupture. Liver- neoplasia, abscess. Pancreas- pancreatitis, neoplasia. Abdominal cavity- peritonitis.
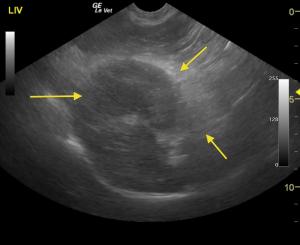
Image Interpretation
The liver in this patient was swollen and mildly irregular in contour. The gallbladder was dilated and egg shaped form with suspended, striating bile, completely inspissated. The wall and neck of the gallbladder was echogenic. Ill defined, inflamed fat was noted in the region. There were minor areas of free fluid was noted as well. Adhesions were noted throughout the region of the portal hilus and enveloped the pyloric outflow. The pancreas presented heterogenous changes in the right limb. The stomach presented some fluid accumulation and mild edema.
Sonographic Differential Diagnosis
Inflamed or possibly ruptured gallbladder mucocele with adhesions in the region of the portal hilus. The common bile duct was not visible owing to adhesion pattern. Free fluid which is suggestive for possible perforation or inflammatory fluid deriving from the pancreas and gallbladder. This is a surgical emergency.
Sampling
Surgical intervention confirmed ruptured GB mucocele and localized bile peritonitis.
DX
Perforated and inflamed Gb mucocele with localized peritonitis and minor pancreatitis
Outcome
Patient underwent an immediate exploratory surgery and successfully recovered









Comments