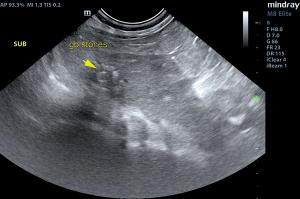
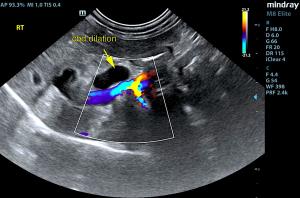
Pain, icterus, elevated total bilirubin and liver values - a bell goes off in every sonographer's head over this combo. Effectively imaging the portal hilus region- including the gallbladder, cystic duct, common bile duct, duodenal papilla, pancreas and pancreatic region- is essential and is exactly how Heidi Putnam, SDEP™ Certified Clinical Sonographer with Animal Sounds Northwest, handled the imaging of this case
The patient is under the diligent care of Dr. Bugarovich of VCA Westmoreland Animal Hospital. Patient is fairly stable on medical therapy post scan; surgery is still being considered an option if patient starts to decline.
Want to learn how to image the critical portal hilus as beautifully and throughly as this, so you can nail down a diagnosis? This view is SDEP Position 13, standard in the SDEP protocol and taught in our labs. For a list of our remaining 2019 labs, click here. Our 2020 lecture/lab dates will be available soon.
DX
Common bile duct calculus. Post hepatic obstruction with chronic cholangitis. Mild potential for common bile duct neoplasia with post hepatic obstruction and hepatic remodeling.
Outcome
Surgical intervention is recommended in this patient with expectations towards bile duct redirection and removal of the calculus. However, the last 2.0 cm of the common bile duct does not look healthy owing to chronic inflammation and likely stricturing. There was no overt evidence of neoplasia; however, there is a minor potential for distal common bile duct neoplasia, yet not suspected.