Everyone loves a great mushroom... unless it's the poisonous kind of Amanita of course. Ever wonder how mushroom toxicity presents clinically and sonographically? Well, Animal Sounds Northwest's (Eugene, Oregon http://www.animalsoundsnw.com/ ) rock star sonographer Amanda Lacey imaged this young Aussie that presented for fulminant liver failure. See what the probe and needle showed on this transcontinental community effort to save this dog, and what happened between Amanda's probe at Dr. Eric Glaze's & Dr. Ken Fletcher's Albany Animal Hospital in Oregon, Lindquist's diagnosis and direction from Sparta, NJ in real-time, Oregon State's tempestive same day medical intervention in Corvallis, Oregon, and the will of this young Aussie dog to overcome those mushrooms that he never should have eaten. This round mushroom was overcome by our "flat world" of technology and effort. (https://en.wikipedia.org/wiki/The_World_Is_Flat)
Image Interpretation
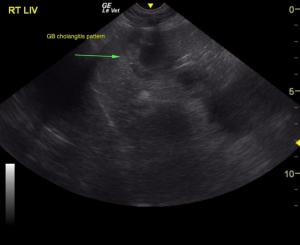
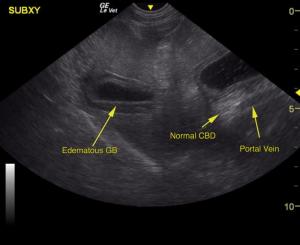
The spleen was volume contracted. The liver was swollen and hypoechoic with a double layered gallbladder. The stomach presented fluid accumulation. The small intestine was unremarkable. There was no evidence of a foreign body. The pancreas was largely uniform with minor, heterogenous changes noted in the right limb. This is consistent with pancreatitis. Surrounding free fluid was noted in the abdomen. Rapid view of the heart revealed volume contraction and shocky contractility.
Sonographic Differential Diagnosis
Acute hepatitis/cholangitis pattern. Free fluid, potentially owing to neoplasia or portal hypertension. Based on the ultrasound results, treatment for gastritis, cholangiohepatitis and pancreatitis would be recommended in this patient. Leptospirosis or toxin exposure is possible. Plasma expander +/- plasma transfusion would be ideal. No complication to FNA was noted. Volume contracted heart with shocky contractility. Very guarded prognosis depending upon underlying cause.
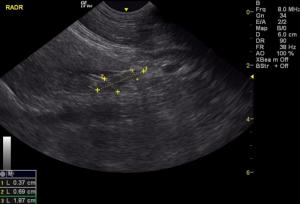
Sampling
Ultrasound-guided FNA of the liver was performed without complication. Cytology results: Mild vacuolar degeneration with suggested regeneration Comment: The mild vacuolar change noted could be associated with a toxic event as suggested. No evidence of underlying disease was detected and overt inflammation was not observed.
DX
Acute hepatitis/cholangitis pattern. Free fluid, potentially owing to neoplasia or portal hypertension.
Outcome
On subsequent referral to Oregon State University, it was determined that the patient did indeed suffer from mushroom toxicity (specifically, one of the genus Amanita, which were found in the patient's backyard and appeared to be partially eaten). Treatment consisted of supportive care and reducing neurotoxins produced in the GI tract. The patient's treatment plan included Denamarin, Lactulose, Cerenia and Omeprazole and a diet of Hill's L/D. Repeated chemistry panel on 10/29/15 and again on 11/23/15 showed progressive decreases in the levels of BUN, GGT and ALKP until normals were attained.